The Future of Behavioral Health

Did you know that there has been a global, mental, and behavioral health crisis long before COVID-19?
According to Our World Data, as of 2017 at least 300 million people were struggling with depression, 284 million with anxiety and 178 million+ with alcohol or drug addiction.
In fact, 1 in 4 people experience significant behavioral illness at some point in life (World Health Organization).
The COVID-19 pandemic made this mental health crisis worse.
As anxiety, depression, and other types of disorders continue to spike, it has created a socioeconomic burden on society. Studies have projected:
- A $210.5 billion cost to the global economy each year from major depression alone (Journal of Clinical Psychology)
- The direct and indirect costs of behavioral illness to a total of approximately 4% of global GDP, exceeding the burden of cancer, diabetes, and respiratory disease combined (National Institute of Mental Health)
- A $16 trillion negative impact on the global economy from 2020–2030 if this crisis isn’t addressed (The Lancet)
To best serve the needs of people worldwide, we must come together to innovate and find solutions that improve health, reduce health care costs, and a create stronger, healthier, and more productive society/workforce.
So, what does the future of behavioral healthcare look like?
According to Deloitte Insights, the future looks bright.
Let’s dig deeper to understand current challenges, and what key players in the pace are doing to seize opportunities and help address this global crisis.
Barriers to Improving Behavioral Health
Government policymakers along with healthcare insurers, providers, and employers are all investing in resources to address this ongoing crisis.
Despite these efforts, there are four challenges that impede being able to fully improve behavioral healthcare. Those four challenges include:
- Gaps in clinical and scientific knowledge: Understanding behavioral health disorders is still in an emerging phase. Consumers are often recommended treatments on a trial-and-error basis and as a result, they are often unclear about the actions they need to take to address their behavioral health – making, disorders overall difficult to categorize, diagnose and treat.
- Stigma and drivers of health: Many times, consumers facing mental and behavioral health issues face stigma making them less willing to seek treatment or to share information with clinicians. Additionally, drivers of health (i.e., access to healthy foods, steady income, and a place to live) can contribute to illness, making it harder for consumers to seek care and fully integrate themselves into society.
- Ineffectual and sub-scale care systems: Less than 1% of government health expenditures (world-wide) goes to mental health services. This is in addition to the shortage of mental and behavioral health professionals were facing. Even though telehealth and app-based access to behavioral health support is continuing to grow, there is still a huge need for diagnosis and care to be accessible and integrated with all medical services.
- Siloed health care data management: Data sharing across various data sources isn’t perfect causing the sources for behavioral health information to be interoperable to support clinicians’ decision-making. Even when the data is shared, many times it’s not usable by everyone because data is not interoperable across users and systems.
6 Disruptive Factors that Will Create Change
Factoring in most trends in the behavioral health landscape, there are 6 disruptive factors that have potential to drive change.
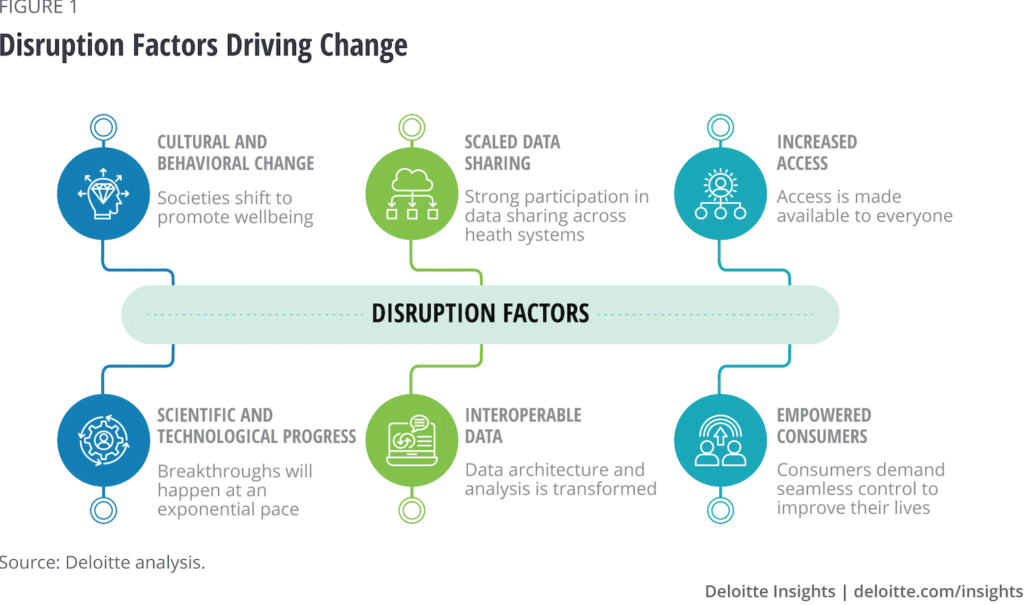
- Cultural and behavioral change: 60% of U.S. adults ages 18-25 view seeing a behavioral health professional as a sign of strength vs. 35% of adults ages 26+, according to the Anxiety and Depression Association of America. With these numbers in mind, the stigma about the behavioral health illness is expected to lessen. To support this, governments are helping lower stigma by increasing investment in behavioral health. They are creating public discussions and enacting policy that integrates population-level behavioral health. On the other hand, employers are emphasizing the importance of behavioral health, and are seeking to serve the needs of employees and their families.
- Scientific and technological advancement: Behavioral health specialists and researchers are beginning to explore the foundations of behavioral health to get greater understanding of genetics, neuroscience, endocrinology, and other relevant fields. New treatments are expected to be cost-effective and improve treatment efficacy. Organizations and providers will be able to tailor treatments based on an individual’s personal needs and genetic profiles. Some of this is already being done by the Qatar Biobank and Qatar Genome Programme with a goal to identify major depressive disorder biomarkers.
- Increased access to care: It is believed that cultural change and cost-effective scientific breakthroughs will lead to better access to care for all. According to MarketWatch, the global health care mobility solutions market is expected to grow 28.4% from 2018 to 2025 to $51 billion, indicating growth in direct-to-consumer behavioral health care solutions. With COVID-19 still around, consumers are still willing to share their data as they engage in telehealth. Meanwhile, with increased awareness of racial behavioral health disparities and unequal access to care, organizations are starting to develop behavioral health resources tailored to minority communities. AI also plays a role in access to care by triaging patients and delivering customized solutions based on individual needs (i.e., automated reminders, flagging intervention needs in chronic disease patients etc.)
- Data sharing: Thanks to the COVID-19 pandemic, consumers are more willing to share data. It is predicted that in the future, consumers will have the capability to systematically access and control all their data within a safe data environment guaranteeing privacy and data blinding. By increasing data sharing, organizations and providers will be better informed of the current state of a person, allowing for proactive identification of potential behavioral health issues before they rise.
- Interoperable data: It is predicted that data sharing will be underpinned by interoperable data built on universal standards and carried on a personal, longitudinal life record. This record will collect data (i.e., holistic, lifestyle information etc.) to help identify issues and opportunities with comorbidities. Standardizing health platforms and electronic health records will help enable the aggregation of data lakes. Organizations will then apply AI to this data to predict early behavioral disorders and recommend interventions to improve outcomes. Currently, Apple, Amazon, Google, and Microsoft support data interoperability in health care by publishing open-source, cloud-based software solutions.
- Empowered consumers: With all these upcoming changes, it is believed that consumers will gain more access to high-quality care while having increased control over treatment modalities. Consumers will have the opportunity to choose highly personalized health tools for self-care, gaining the opportunity to sustain their health independently. Additionally, they will have the ability to evaluate providers prior to treatment, choose services outside of the traditional services offered (i.e., telehealth), monetize data if they choose too etc. – resulting in providers and organizations becoming more consumer-centric.
Opportunities Disruption Factors Will Create
The 6 disruptive factors we previously discussed are powerful trends that can create change.
However, for change to happen, key players across the mental and behavioral space must take the necessary steps to make this a reality and seize all possible opportunities.
Let’s explore some steps key players can take.
Public and Private Insurers
Both public and private insurers should consider:
- Focusing on building plans that offer mental and behavioral health support on holistic, and preventative care for all members.
- Gaining more access to consumer data (i.e., health, social, economic, and environmental – at an individual and population level). With the information collected, insurers will be able to analyze the data to pinpoint behavioral health insights while getting a deep understanding of the drivers of health and clinical symptoms of behavioral diseases.
- Developing customized behavioral health plans that support proactive care and prevention built from data and analytics from members.
- Creating cross-sector collaboration to blend different types of data (i.e., social media, consumer spending etc.) to improve consumers behavioral health.
- Broadening the types of behavioral health care networks offered to members. This includes finding creative ways to reimburse providers for a wider array of preventative behavioral health services. This is necessary to expand access to care while supporting business models that leverage the array of potential provider types, new technology systems, predictive information, personalized interventions and more.
Care Providers
Care providers should consider:
- Gaining access to consumer data (i.e., apps, wearables etc.) and applying analytics to best understand patients’ behavioral health. This will allow providers to create and deliver preventative, customized care solutions supported by advanced predictive modeling and analytics.
- Leveraging emerging technology for interventions occurring in both inpatient and outpatient settings. For this to be successful, providers will need to systematically incorporate technology into care delivery at every step of their patient’s journey. Some technology options include self-guided, gamified treatment to virtual assistants. AI also ensures better care for patients through enhanced digital triage processes, augmented and virtual reality treatments, computational psychiatry to name a few.
- Augmenting workforce capacity via community and in-home behavioral health care to ensure patients receive treatments as soon as possible.
- Value-based financing models which compensate providers based on the overall quality of care.
Employers
Employers must build on the disruptive factors to build a future that meets the needs of employee’s behavioral health. This will allow employers to become more competitive as they’re helping employees thrive.
Employers should consider:
- Introducing customized products/services that integrate behavioral health treatments into employees work lives. These treatments should focus on more than just prevention, it should help increase employee’s acuity, acumen, abilities, ethics, and social capacities. Data from these efforts can also be collected for employers to analyze and understand/support employee needs.
- Incorporating employee assistance programs that offer high-quality, behavioral health support that allow employees to pursue their well-being holistically.
- Demonstrating employees (by assuring them) that engaging with their behavioral health at work will not harm their career trajectory.
- Appointing an ethics and health data protection officers to manage and protect employee data.
- Partnering with experts to help plan, manage and implement all new benefits and services (if this is new to the employer).
Government Policymakers
Government policymakers play a critical role in getting key players to collaborate and work together to seize opportunities and create change.
Their role also involves building trust amongst these players as well as the public.
With that said, government policymakers should consider:
- Prioritizing new investments in behavioral health solutions (local and on a national level).
- Ways to systematically enable monitoring and care by leveraging new technology. This includes creating expansive licensing requirements for mental and behavioral health specialists that allow them to leverage telehealth to work on a national and international level. Additionally, government policymakers will need to work with other industry key players to ensure that there is government-sponsored support for the shifting reimbursement models required to support the future of behavioral health.
- Creating organizations that support and help manage the ethical and regulatory areas that exist within the behavioral health space. Government policymakers should also consider regulations that guarantee that corporations don’t discriminate against individuals based on their behavioral health.
Closing Thoughts
As you can see the future of behavioral healthcare is positive.
Change has begun to accelerate thanks to 2020 and other challenges the industry has been facing.
To create business value and improve the health and wellness of societies worldwide, we must all come together to take advantage of the trends, consumerism, data, technology use and other insights to create solutions and business models that can transform and improve behavioral healthcare for the long run.
To find work or discuss your organizations staffing needs, complete the form or call us at (305) 974-1538 to speak with a MASC Medical staffing and recruiting expert.