Is There a Mental Health Crisis in America?

Is there a mental health crisis in America?
Over the past year, this question has been asked occasionally due to the COVID-19 pandemic and rise in people reporting mental health issues.
However, did you know that even before the COVID-19 outbreak, 19% (or 47.1M) adults experienced a mental illness? According to Mental Health America’s (MHA) 2021 State of Mental Health in America report, this is an increase of 1.5M people over last year’s report.
To get a glimpse and best understand the mental health state in America, we’ve extracted some key takeaways from the 2021 MHA report:
Overall Major Findings –
- Suicidal ideation among adults is increasing by .15% (or over 460,000) people from last year
- 24% of adults with a mental illness report an unmet need for treatment (this number has not declined since 2011)
- 7% of youth in the U.S. have severe major depression; this rate was highest among youth who identify as more than one race at 12.4%
- 60% of youth with depression do not receive any mental health treatment; even in states with the greatest access 1 in 3 are going without treatment
- Even among youth with severe depression who receive some treatment, only 27% receive consistent care
- 8% of Americans with a mental illness are uninsured; this increased for the first time since the passage of the affordable care act
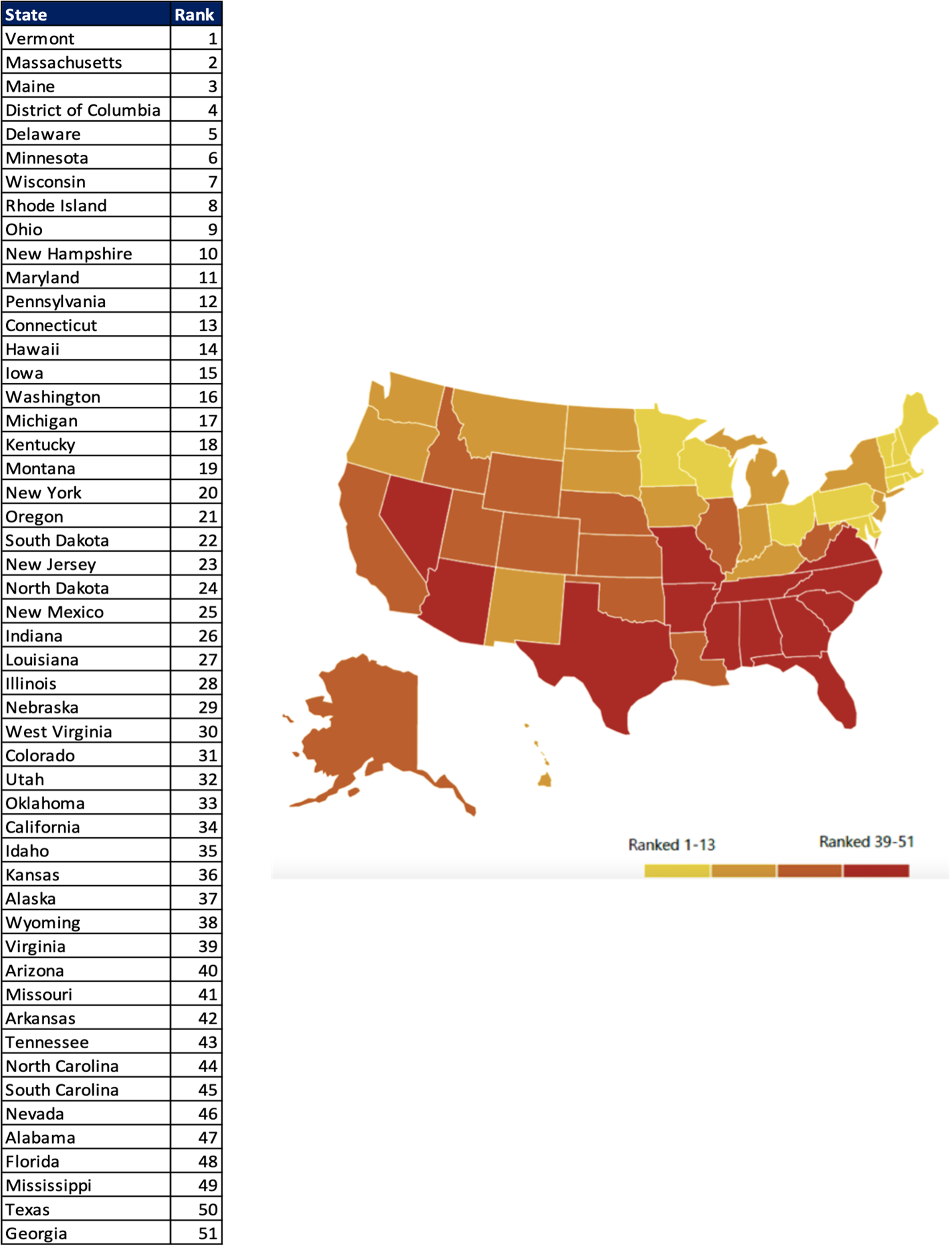
Overall Ranking of Both Adult and Youth Measures as well as Prevalence and Access to Care Measures –
From this chart, we can see the overall ranking (scores) for each state.
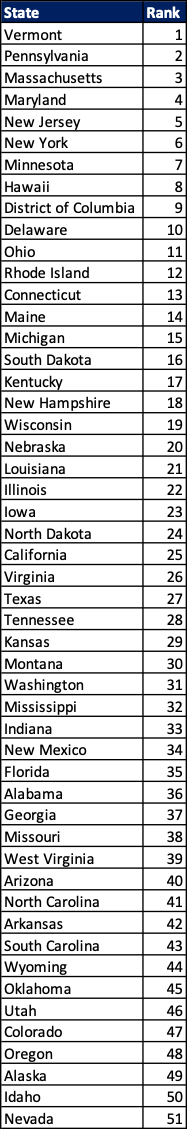
A ranking of 1-13 indicates lower prevalence of mental illness and higher rates of access to care while a ranking of 39-51 indicates higher prevalence of mental illness and lower rates of access to care.
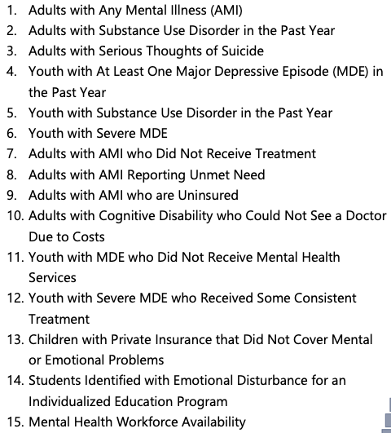
The combined scores of all 15 measures (as defined below) make up the overall ranking:
States with the largest changes in overall ranking included: Colorado, Montana, Washington, Missouri, Kansas, and Iowa.
Prevalence of Mental Illness Ranking –
From this chart, we can see the prevalence ranking (scores) for each state.
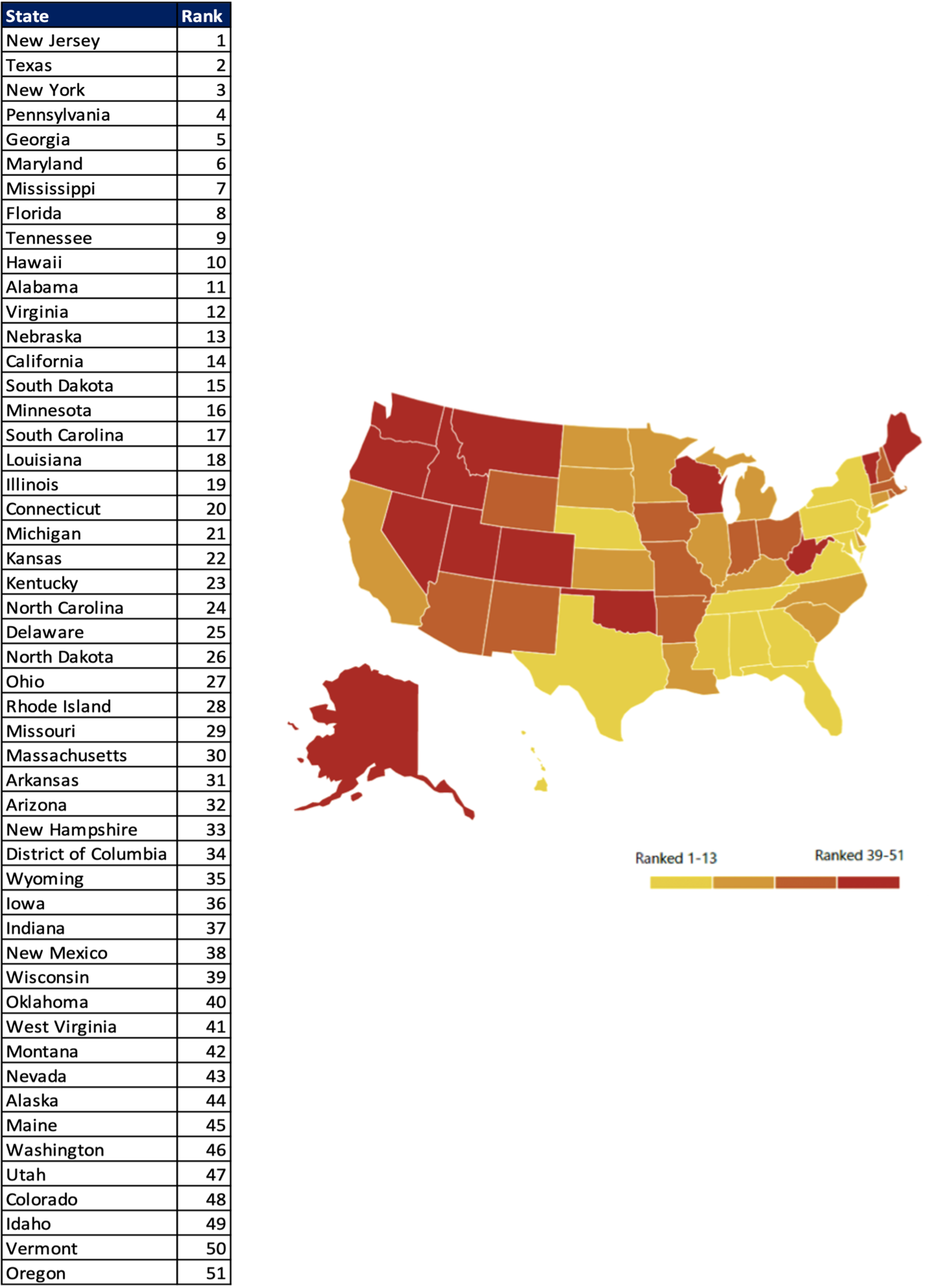
A ranking of 1-13 indicates a lower prevalence of mental health and substance use issues vs. states that rank 39-51.
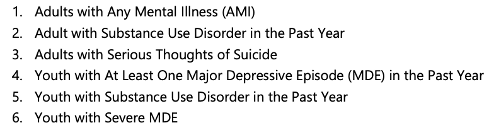
The combined scores of all 6 measures (as defined below) make up the prevalence ranking:
States with the largest changes in need/prevalence ranking included: Oklahoma, North Carolina, South Dakota, Tennessee, and Massachusetts.
Access to Care Rankings –
From this chart, we can see the access to care ranking (scores) for each state. The access to care ranking demonstrates how much access to mental health care exists within a state. In other words, the access measures include access to insurance, treatment, quality and cost of insurance, special education, mental health workforce (ADD LINK TO Types Of Mental and Behavioral Health Professionals ONCE LIVE) availability etc.
A ranking of 1-13 indicates that a state provides relatively more access to insurance and mental health treatment.
The combined scores of all 9 measures (as defined below) make up the access to care ranking:
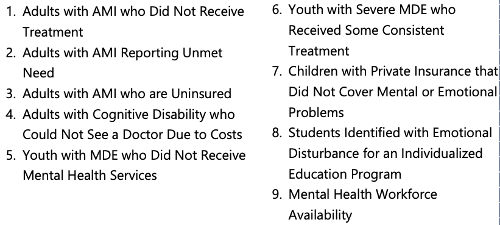
States with the largest changes in access to care ranking included: Missouri, Colorado, Louisiana, and Kentucky.
Adult Prevalence of Mental Illness Key Facts –
- 19% (or 47M) adults are experiencing a mental illness
- 67% of adults reported having a substance use disorder in the past year
- 34% (or 10.7M) adults reported serious thoughts of suicide – an increase of over 460,000 people from last year’s report
Youth Prevalence of Mental Illness Key Facts –
- 84% of youth ages 12-17 reported suffering from at least one major depressive episode (MDE) in the past year – an increase of 206,000 youths from last year’s report
- 83% of youth reported a substance use disorder in the past year
- 7% (or 2.3M) youth cope with severe major depression – an increase of 126,000 youths from last year’s report
Adult Access to Care Key Facts –
- 57% (or 26M) adults with a mental illness receive no treatment
- 86% of adults who did not receive mental health treatment were covered by health insurance, indicating that ensuring coverage is not the same as ensuring access to care
- 6% of adults with a mental illness reported that they were not able to receive the treatment they needed, demonstrating they face the same barriers that contribute to the number of individuals not receiving treatment:
- No insurance or limited coverage of services
- Shortfall in psychiatrists and an overall undersized mental health workforce
- Lack of available treatment types (inpatient treatment, individual therapy, intensive community services)
- Disconnect between primary care systems and behavioral health systems
- Insufficient finances to cover costs including co-pays, uncovered treatment types, or when providers do not take insurance
- 8% (or 5.1M) adults with a mental illness are uninsured
- 69% of adults with a cognitive disability were not able to see a doctor due to costs
Youth Access to Care Key Facts –
- 6% of youth with major depression do not receive any mental health treatment
- 3% of youth with severe depression receive some consistent treatment
- The rate of children with private insurance that does not cover mental or emotional problems decreased by 0.3% from last year’s report; however, there are still 901,000 youth without coverage for their behavioral health
COVID-19 and Mental Health –
The COVID-19 pandemic had a disastrous effect on the mental health of the entire nation.
We can all agree that the risk of contracting the virus alone caused a traumatizing event for everyone. But in addition, COVID-19 led to change in our physical and social environments which led to greater rates of isolation, loneliness, financial hardship, housing and food insecurity and interpersonal violence – all affecting the mental health crisis in the nation.
In 2014, MHA created an online screening program which includes a collection of ten free, anonymous, confidential and clinically validated screens that are among the most commonly used mental health screening tools in clinical settings.
Overall, through September 2020, over 6M people have taken a screen. More specifically from January to September 2020 (during the peak of COVID-19), approximately 1.5M people have taken a screen. The screening results allow MHA to collect national mental health information in real-time, allowing them to recognize and react to changes in the mental health of the nation, including the mental health crisis throughout the COVID-19 pandemic.
Here are some key findings from the data collected from approximately 1.5M screeners from January to September 2020:
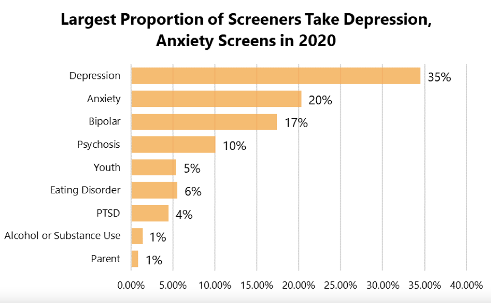
The top 3 screens taken were for depression (35%), anxiety (20%) and bipolar (17%). 73% of screeners identified as female, 25% identified as male and 2% identified as another gender.
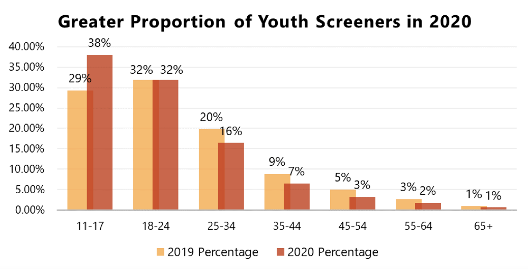
As you can see, 38% of screeners were youth ages 11-17, a 9% increase over 2019. This indicates that in 2020, youth under the age of 18 were actively searching for mental health resources and support. 18–24-year old’s stayed the same from 2019-2020 at 32%.
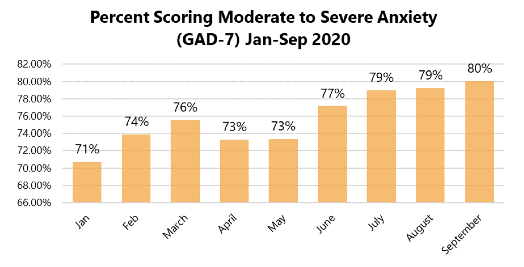
From January to September 2020, approximately 315K people took the anxiety screen, a 93% increase over 2019. In September 2020:
- An average of 2,262 anxiety screens were taken per day
- 80% of people who took an anxiety screen scored for moderate to severe anxiety with 48% scoring for symptoms of severe anxiety
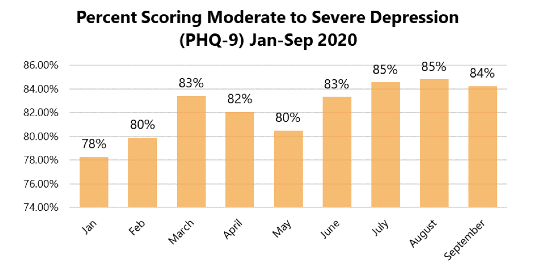
From January to September 2020, approximately 534K people took the depression screen, a 62% increase over 2019. In September 2020:
- An average of 4,321 depression screens were taken per day
- 84% of people who took a depression screen scored for moderate to severe depression, with 31% scoring for symptoms of severe depression
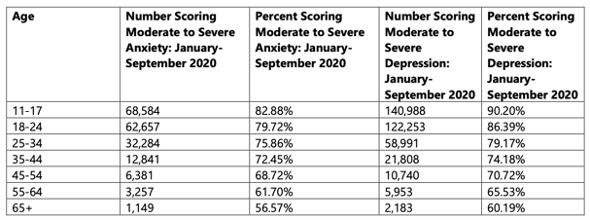
Throughout the COVID-19 pandemic, youth ages 11-17 were more than likely than any other age group to score for moderate to severe symptoms of anxiety and depression.
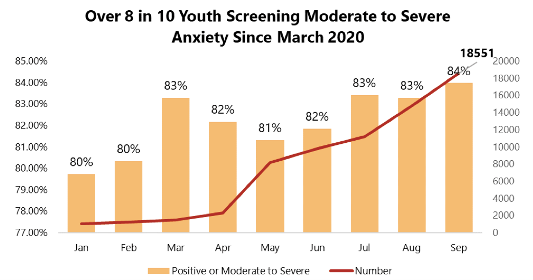
Over 80% of 11–17-year old’s who took an anxiety screen scored for moderate to severe anxiety. That percent increased to 84 in September 2020.
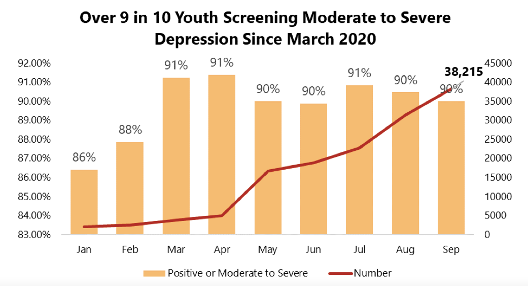
At least 90% of 11–17-year old’s who took a depression screen scored for moderate to severe depression. That percent remained the same in September 2020.
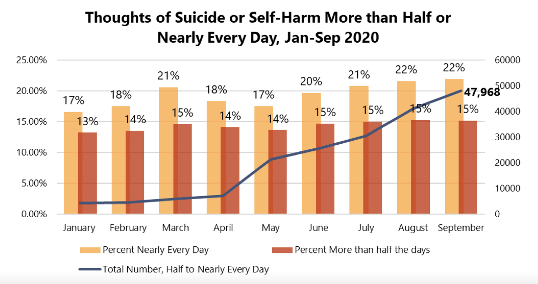
Since the COVID-19 outbreak (March 2020), over 178,000 people have reported frequent suicidal ideation. In September 2020, 37% of people screened for depression indicated they experienced suicidal ideation more than half or nearly every day of the previous two week. 22% indicated that they experienced thoughts of suicide or self-harm nearly every day.
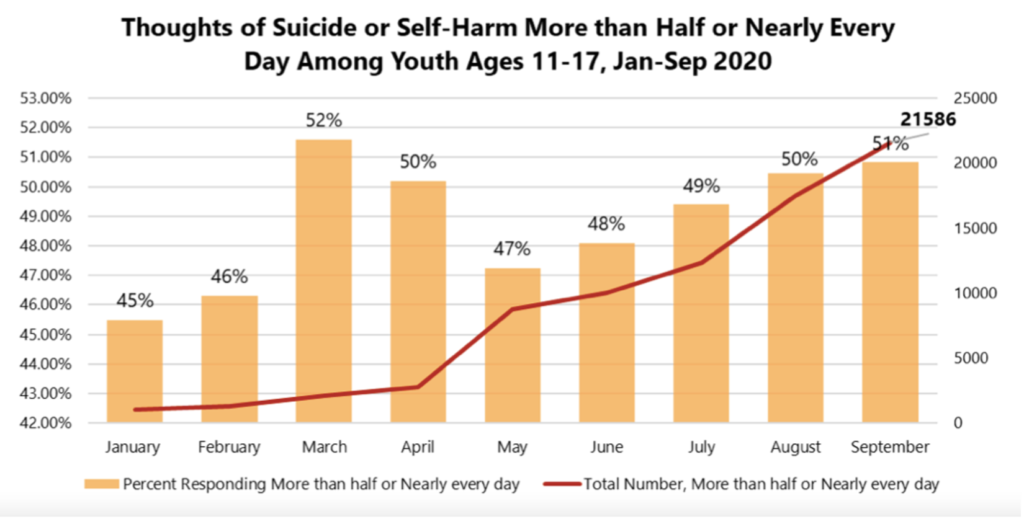
In September 2020, 51% of 11–17-year old’s reported having thoughts of suicide or self-harm more than half or nearly every day of the previous two weeks. From January to September 2020, 77,470 youth reported experiencing frequent suicidal ideation, including 75,107 since the beginning of the pandemic in March 2020.
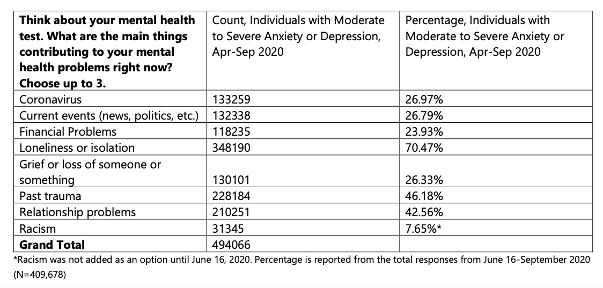
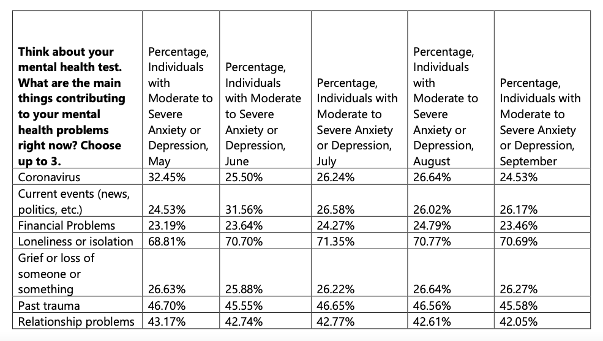
Main Concerns of People Screening Positive for Mental Health Conditions
As we can see, this report not only confirms that there is a mental health crisis in America, but that it isn’t getting any better.
We must remember that as a nation, it is our responsibility to create initiatives to help combat the mental health crisis. We hope that this MHA 2021 report synopsis has given you a complete picture of the mental health state in the U.S. Together lets help tackle this crisis.