COVID-19 Impact on Psychiatric Care

COVID-19 has affected psychiatric care across the world.
From our is there a mental health crisis in america? blog, we know that America has been undergoing a mental health crisis even prior to the COVID-19 pandemic.
The pandemic not only affected society in general, but it disrupted the entire U.S. healthcare system.
Here are some key highlights from a Psychiatry Research study to understand how COVID-19 affected psychiatric care. More specifically on access to care, quality and the way health care services were being provided.
Impact on Psychiatric Care in Outpatient, Inpatient, Emergency Room, Consultation Services & the Community
According to the American Psychiatric Association (APA), there has been many changes when it comes to delivering care. Everything from legal doctrines and privacy rules have been bypassed to provide care in a different environment. The APA’s national COVID-19 practice guidance table best represents this.
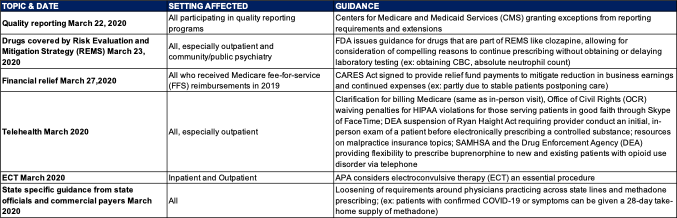
Let’s further analyze the changes that have occurred according to the psychiatric care setting.
In outpatient settings, the biggest changes occurred thanks to telehealth. When the pandemic outbreak first occurred, the U.S. government temporarily waived numerous regulations as well as regulatory barriers to allow for various platforms to be used nationwide. Remote consultation via telemedicine began and it is still used today, worldwide.
On the other hand, inpatient settings are more challenging due to the physical structure of the psychiatric units and modalities in which care is delivered. To help minimize COVID-19 exposure and contraction, no visitor policies and suspension of group activities were implemented in a few facilities as well as the tightening of admission criteria.
Lastly, when it came to consultation services, hybrid models were implemented to leverage all available resources. Plus, triaging, and determining whether patients were going to be seen in-person, via phone or video. In several hospitals, consultation services are still being provided remotely.
Effects on Psychiatric Clinicians
The COVID-19 pandemic not only affected Americans but also healthcare providers.
When the pandemic occurred, clinicians experienced stress, anxiety, and fear. All of this resulted from:
- Seeing what was happening worldwide (mortality rates, hospitalizations)
- Adapting to the changes happening at work (new protocols)
- Not having enough PPE
- Being exposed and exposing their families to the COVID-19 virus and possibly having to quarantine
- The need for psychiatric treatment increasing
- Having to take longer work shifts
- Lack of knowledge and training on how to treat the COVID-19 virus
Additionally, when it came to providing psychiatric care, psychiatric clinicians were affected ethically and financially. For example, they’ve had to:
- Put clinical research on halt
- Cancel or postpone medical conferences
- Pull residents from psychiatric rotation trainings to work in COVID positive settings
- Transition didactic education, supervision, and outpatient visits to virtual
- Deal with a few medical students deciding not to physically attend clinical rotations
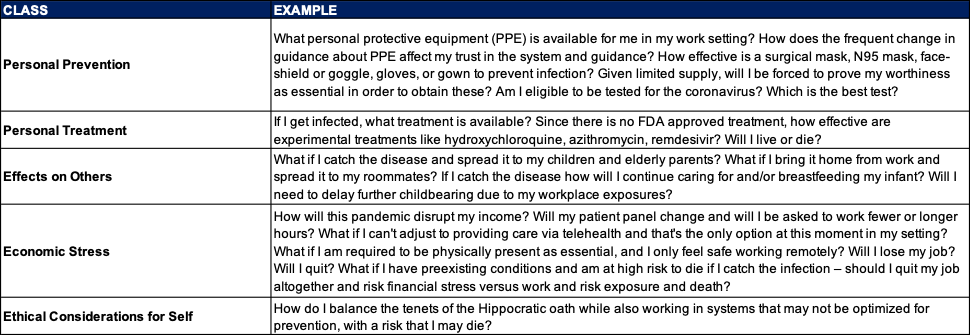
Across various settings, psychiatric clinicians and other members of the healthcare team have had concerns when it came down to COVID-19.
Here is a detailed chart that explains the specific concerns of psychiatric clinicians across the country during the COVID-19 pandemic:
Ethical Challenges in an Evolving Crisis
Psychiatric care, treatment and the overall environment is different when compared to other medical specialties.
Psychiatric units are not set up to maintain infection control. In fact, psychiatrists and other members of their team typically don’t wear protective gear. Most patients are ambulatory and accustomed to socializing in communal spaces. Patients with severe psychiatric symptoms may find it difficult to follow simple precautions (i.e., hand washing, social distancing, wearing masks etc.)
For inpatient psychiatric treatment to be effective much depends on interaction. Therefore, when the COVID-19 outbreak began, much of this was in conflict. Throughout the pandemic, there has been frequent and severe outbreaks occurring on psychiatric units with some outbreaks leading to multiple COVID-19 related deaths. Knowing that the risk of contracting COVID-19 is high for hospitalized psychiatric patients, withholding information without a patient’s knowledge or consent is ethically unacceptable except in emergency situations according to the American Medical Association. Patients should have the right to know the risk that comes with being hospitalized during a pandemic.
Telepsychiatry evolved during the pandemic. While this is a great option to reduce the risk of infection, at the beginning there was a security issue since telepsychiatry didn’t meet privacy standards set by the Health Insurance Portability and Accountability Act (HIPAA). Later, to allow for patients to continue to get care with low risks of contracting COVID-19, federal policy allowed for the use of telehealth in general despite risks to patient privacy.
As we can see, in addition to all the challenges that psychiatrists have been facing, they have faced complex ethical challenges and resource limitations.
The Evolution of Psychiatric Care
The COVID-19 pandemic was something no one expected nor planned for.
We lost a lot of lives.
Healthcare providers have been and are still burned out.
People are afraid, stressed and undergoing mental health issues like never before.
Despite all the challenges, the pandemic has also allowed for psychiatric care to evolve.
Let’s look at what specific psychiatric settings have done to adapt and continue evolving:
Outpatient Psychiatric Care
Outpatient psychiatric care now includes several virtual modalities.
Healthcare systems leveraged the use of telehealth to continue to provide access to care to patients. For a few people, this involved having to learn how to utilize webcam-based programs either through their computers, smartphones, or tablets. Telephone based encounters also occurred. Both becoming the new standard of care.
While telehealth was a positive trend during the pandemic, some patients became fearful of initiating medication trials without an in-person encounter with their physician. Especially, since a few psychotropic medications require bloodwork. This increased their fear and concern of having to visit a medical facility, where they could possibly contract the COVID-19 virus. To address some of these issues, hospitals, clinics, private practices etc. began to screen patients for COVID-19 symptoms prior to having them enter their facilities.
In addition, patients with substance use disorders (SUDs) were extremely vulnerable to the COVID-19 pandemic due to their compromised pulmonary system and socioeconomic status. With this is mind, national organizations and states began to provide guidance around prescribing medication to SUD patients. Associations such as the substance abuse and mental health services administration (SAMHSA) and the drug enforcement agency (DEA) issued guidelines right around when the pandemic first broke out. More specifically, they loosened restrictions to allow methadone to be prescribed in higher quantities, suboxone to be prescribed via phone, and controlled substances to be e-prescribed directly to pharmacies.
Since the start of the pandemic, there was a lot of concern for older adults due to their high risk of mortality if COVID-19 was contracted as well as mood destabilization because of social distancing and shelter in place guidelines. Older adults became fearful (in fact, some still are) about the possibility of getting COVID-19, and some even decided to quarantine in their homes. As a result, some older adults now suffer from anxiety and depression because of social isolation and loneliness. To address this issue, telepsychiatry became available and it was also recommended that family members and caregivers assist in the delivery of their care.
Lastly, healthcare providers working in outpatient settings had to transition to providing outpatient care while working from home and providing staff training virtually. Some of these things are still intact today; however, in-person visits and consultations are starting to come back as we enter the post-pandemic era.
Emergency Room Psychiatric Care
During the COVID-19 pandemic, emergency rooms saw an increase in psychiatric visits because patients were having a hard time getting in contact with their therapists and/or psychiatrists.
Additionally, patients seeking or being referred for emergent psychiatric evaluations also had an impact. Facilities across the nation implemented screening protocols (question based) to triage patients for risk of exposure to COVID-19 and to assess their symptoms. This evolved throughout the pandemic. At the beginning, only patients who showed high risk of exposure and symptoms of COVID-19 were immediately tested for COVID-19. Nowadays, if a patient is referred for inpatient psychiatric admission, they are immediately given a rapid COVID-19 test prior to being evaluated by a psychiatrist and being admitted to an appropriate unit.
As previously mentioned, patients and people in general have developed this fear of contracting the COVID-19 virus. While healthcare systems are conducting rapid tests, they are also offering patients the opportunity to consult with a physician via telephone. Other select evaluations can also be done by phone.
And lastly, if patients need to be evaluated in person, physicians and patients are following social distancing guidelines plus the use of masks etc. To help mitigate the risk of infection among healthcare staff, some healthcare systems have transitioned to a shift work model.
Inpatient Psychiatric Care
Providing care to patients in an inpatient psychiatry setting during COVID-19 has changed to maintain social distancing protocols and guidelines.
This alone was a challenge since part of the treatment for patients in this type of setting includes close contact, group therapy sessions, eating meals together, sharing bathrooms, sleeping rooms (if partially hospitalized), having family close to help with recovery or treatment etc. Despite this, leadership at many inpatient psychiatry settings focused on making the necessary changes to keep patients and staff safe by working together, communicating, and coming up with the best solution to accomplish this. Here are some changes that occurred:
- Screening, re-screening, PPE, use of designated clothing, cleaning of surfaces, disinfection etc. were implemented to prevent the spread of COVID-19
- Medical student(s) visits were minimized
- Back-up pools and job reassignments for physicians were created (as needed)
- Isolation rooms in psychiatric inpatient units were created
- The number of visitors were restricted
- The criteria for psychiatric admission was tightened
- Changes to group therapy sessions (i.e., limiting the number of participants, utilizing social distancing) were implemented
All these changes were put into action to keep people safe and reduce the risk of infection.
But, with that came some isolation as patients are limited to the types of treatments they can receive, increasing the possibility of psychiatric hospitalizations in the future.
Psychiatric Care on the Consultation-Liaison Service
Psychiatric care on the consultation-liaison service means care is provided for patients in the emergency room and in an inpatient medical setting.
In the emergency room, consultation-liaison services started using virtual methods to provide care. But, in some cases, hospitals continued to see patients in the emergency room and obstetrics floor depending on the severity of the case, with the appropriate use of PPE.
Consultation-liaison psychiatry in inpatient settings includes patients that have been hospitalized for prolonged periods of time. Their goal is to support patients to understand their medical illness and help them in the recovery process. Most patients in these types of setting have chronic illness, making them a high risk to COVID-19. As in other healthcare settings, virtual evaluations were emphasized to reduce the risk of cross contamination and exposure, but in-person interactions also occurred for psychiatric emergencies – creating a hybrid model of care.
Psychiatric Care in the Community
Within the community there are patients with serious mental illnesses.
These patients have a high risk of COVID-19 morbidity and mortality due to their medical risk factors, lack of good hygiene habits, homelessness and living situations. During the pandemic, psychiatrists needed to adjust the way they deliver care to these patients.
Throughout the nation, select state-supported community behavioral health organizations and programs of assertive community treatment developed COVID-19 response protocols for various settings such as shelters, mental health group home residences, clinics, home visits, etc. These protocols as we’ve seen in other healthcare settings included a screening where patients were asked specific questions, underwent temperature checks, and possibly isolation, depending on their screening results.
The healthcare providers running these screens wore PPE, utilized social distancing to avoid risk of contraction and at times leveraged the state COVID-19 hotline. For home visits, patients were screened prior to the visit and if the patient was symptomatic, providers could refrain from entering the home.
Many states also implemented policy, regulatory and payment reforms for the provision of remote telehealth, access to residential care staff and medications, and financial support for community-based services.
And lastly, psychiatric residencies were and to date are coming up with creative ways to train residents. Some of these strategies include hosting virtual meetings, self-directed learning and encouraging residents to seek appropriate care when needed.
Conclusion
The COVID-19 pandemic has disrupted mental health services in 93% of countries worldwide, according to the World Health Organization.
As the pandemic continues, it is increasing the demand for mental health services. People are experiencing bereavement, isolation, loss of jobs (income), fear, all which trigger mental health conditions (i.e., drug use, insomnia, anxiety, stress, depression) or are exacerbating existing ones.
As we can see COVID-19 has and is still affecting psychiatry in many ways – no matter if you are a patient or healthcare provider. There is still some uncertainty as to where this pandemic is going to take psychiatric care in the long run.
But we must remember that with all the challenges came solutions and as we continue to evolve, we hope that these insights into how COVID-19 has impacted psychiatric care to date has helped you gain more knowledge to come up with solutions to better the mental health state in America.